Getting clear guidance on Class I medical devices is key in a product’s successful journey to market. To place a medical device on the market in the EU, manufacturers must now demonstrate conformity with the EU 2017/745 Medical Device Regulation (MDR) which has replaced the previous Medical Device Directive 93/42/EEC (MDD) and Active Implantable Medical Devices Directive 90/385/EEC (AIMDD).
To provide advice and assist the Commission and Member States, Medical Device Coordination Group (MDCG) was formed with the aim to ensure harmonised implementation of the MDR. In collaboration with interested parties the MDCG has issued guidance documents in accordance with Article 105 of the MDR with more still to follow. Below is a detailed summary of the steps required before placing a Class I medical device on the market as outlined in the MDCG 2019-15 rev. 1.
Integrate MDR into Quality Management System
To guarantee compliance with all the requirements outlined in the MDR, it is highly recommended that applicable provisions are integrated into the manufacturers QMS to ensure correct assessments and documentation is created to provide evidence of compliance. This includes ensuring a system for risk management is in place and a responsible person for regulatory compliance is in designated.
By establishing an appropriate QMS it will ensure that compliance with general obligations (as established in Article 10) are being complied to in the most effective way, including through internal audits.
Confirm product is a medical device
Article 2 outlines the definitions of the MDR including the term “medical device”. This states that ‘medical device’ means “any instrument, apparatus, appliance, software, implant, reagent, material, or other article intended by the manufacturer to be used, alone or in combination, for human beings for one or more of the following specific medical purposes:
• diagnosis, prevention, monitoring, prediction, prognosis, treatment, or alleviation of disease
• diagnosis, monitoring, treatment, alleviation of, or compensation for, an injury or disability
• investigation, replacement, or modification of the anatomy or of a physiological or pathological process or state
• providing information by means of in vitro examination of specimens derived from the human body, including organ, blood, and tissue donations and which does not achieve its principal intended action by pharmacological, immunological, or metabolic means, in or on the human body, but which may be assisted in its function by such means.
It also deems the following to be a medical device:
• Devices for the control or support of conception
• Products specifically intended for the cleaning, disinfection or sterilisation of devices as referred to in Article 1(4) and those above

Confirm product classification
The classification of medical devices is governed by the intended purpose of the device and their inherent risks linked to duration, part of the body, whether it is active or not and whether it is invasive or non-invasive.
Based on the classification rules outlined in Annex VII, manufacturers should determine which class their medical device falls under; Class I, Class IIa, Class IIb, or Class III. If more than one rule applies, then the highest classification should apply.
Under the MDR some Class I medical devices have now been reclassified, and the classification has been broken down into include Class Im, Class Is and Class Ir meaning present guidelines cannot be applied to devices now in a higher risk class. Manufacturers with devices which are intended to be used in a sterile condition (Class Is), with a measuring function (Class Im) or are reusable surgical instruments (Class Ir), must now apply the procedures set out in Annex IX and have involvement from a notified body as detailed below.
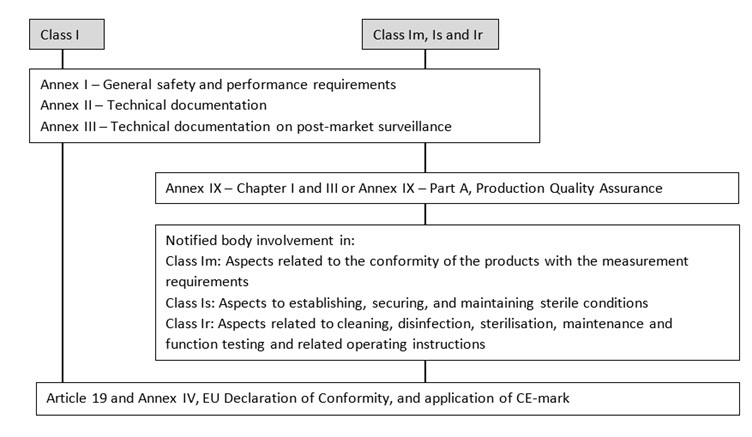
Procedures before placing on the market
To place a medical device on the market several steps must be completed: Meet general safety and performance requirements, conduct clinical evaluation, prepare technical documentation, prepare Instructions for Use and Labelling and request Notified Body Involvement.
Annex I of the MDR specifies the general safety and performance requirements that must be met, considering what applies based on the intended purpose of the device. To ensure traceability and demonstrate conformity to the requirements, a checklist/table should be used to document the applicability of each requirement to the device, the solution to comply with each applicable requirement, reference to any possible CS or harmonised standard and reference to the evidence within the technical documentation.
A risk management system should be established and implemented to allow for identification and analysis of the hazards, estimation and evaluation of the associated risks and elimination or control of residual risks. This should be a continuous process throughout the lifecycle of the product and requires updating regularly (including adopting measures based on information collected from the post-market surveillance).
All devices, regardless of the classification, require a clinical evaluation to be conducted to justify the level of clinical evidence required to demonstrate conformity. The clinical evaluation should be planned, conducted, and documented in accordance with Article 61 and Part A of Annex XIV and should consider the following:
• Available alternative treatment options
• Incorporation of clinical data
• Acceptability of the benefit-risk ratio

If there is not enough clinical data to demonstrate compliance with the MDR, then a clinical investigation may be required. However, devices already certified against the MDD may also use general or clinical post-market follow-up studies to provide the additional information required.
For each device, technical documentation should be prepared and maintained so that it is readily available with records being kept for a period of at least 10 years since the last device covered by the declaration of conformity was placed on the market. Annex II and III lists the particular elements which should be included. This includes the aspects listed above along with the device description and specification, labelling and instructions for use, detailed information on design and manufacturing, verification and validation information and post-market surveillance information.
Appropriate labelling and packaging should accompany each device to identify the device as well as the manufacturer and/or the authorised representative. Class I medical devices do not require instructions for use, as long as they can be used properly and safely without such instruction. The exception to this is mainly posed for Class Ir devices which require reprocessing (cleaning and sterilisation), where the instructions for use should provide data to ensure it is used safely, taking into account the training and knowledge of potential users.
Manufacturers with devices which are Class Im, Class Is and Class Ir can then choose a Notifying Body listed on the NANDO database as accredited for the relevant code and corresponding type of device:
“Devices in sterile condition”: Code MDS 1005
“Reusable surgical instruments”: Code MDS 1006
“Devices with a measuring function”: Code MDS 1010